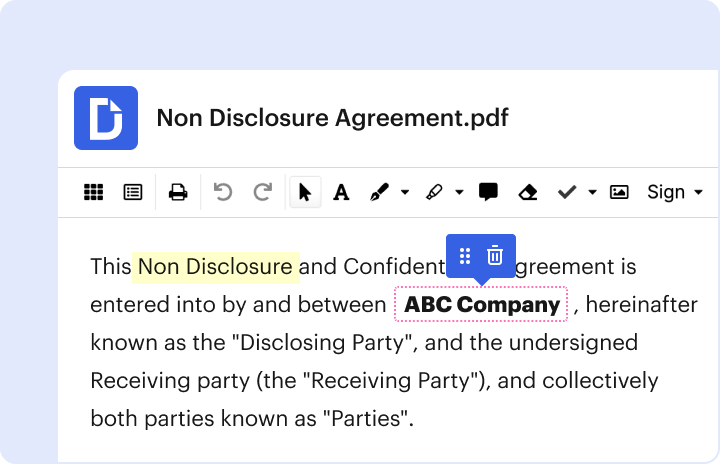
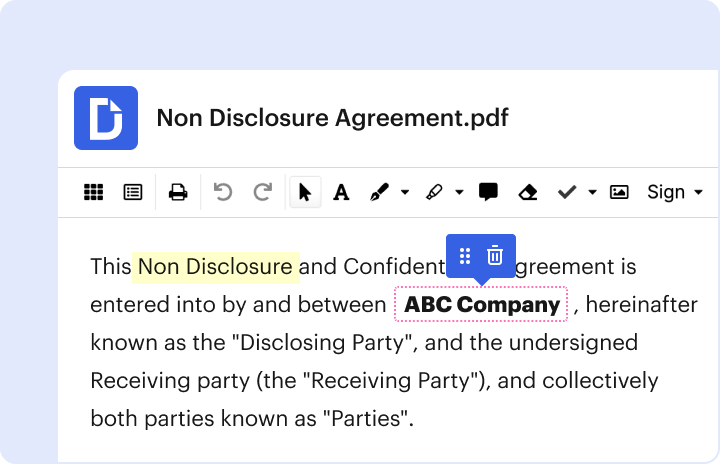
Dochub is the best editor for changing your forms online. Adhere to this straightforward guide to edit Referral authorization form in PDF format online for free:
Discover all the benefits of our editor today!
Fill out referral authorization form onlineWe've got more versions of the referral authorization form form. Select the right referral authorization form version from the list and start editing it straight away!
| Versions | Form popularity | Fillable & printable |
|---|---|---|
| 2018 | 4.9 Satisfied (36 Votes) | |
| 2010 | 4.8 Satisfied (48 Votes) |
We have answers to the most popular questions from our customers. If you can't find an answer to your question, please contact us.
What is the difference between a referral and authorization?A referral is an order from your PCP to see a specialist or receive certain medical services from some providers. Your PCP helps make the decision about whether specialist services are necessary for you. Prior authorization is approval from the health plan before you get a service or fill a prescription.
What is mean by referral in medical billing?A referral, on the other hand, is when a primary care physician (PCP) recommends a patient to a specialist for consultation or healthcare services they are unable to provide. Many insurance companies require this step before agreeing to pay for a visit to a specialist.
What is referral and authorization?The referral certification and authorization transaction is any of the following: A request from a health care provider to a health plan to obtain an authorization of health care. A request from a health care provider to a health plan to obtain authorization for referring an individual to another health care provider.
What is referral medical billing?Seeking assistance from another specialist for additional services and management is considered as a Referral in Medical Billing. The fundamental thing about Referral is that you need to take consent from your primary health care doctor before you take an appointment from another specialist.
What is referral authorization in healthcare?A referral is issued by a primary care physician (PCP) for the patient to see a specialist. In contrast, prior authorization is issued by the payer (an insurance provider), giving a medical practice or physician the approval to perform a medical service.
Referral authorization form pdf TRICARE patient referral authorization form PDF Referral authorization form online Referral authorization form doc Patient referral authorization form TRICARE Patient referral authorization form Humana Military TRICARE east referral form pdf TRICARE east referral request form
What is an INSURANCE Referral? The term Insurance Referral refers to the permission or authorization of your insurance plan that they may require in order to see a recommended specialist, doctor, hospital, or type of treatment.
What is a referral authorization form?A RAF is a referral form used by a Primary Care Provider (PCP) to carry out his/her case management role. It is to be used to refer assigned members for medically necessary services not generally provided by the PCP. Each RAF can only be used once and should contain diagnostic and treatment orders for only one patient.
What is authorization in healthcare?Definition of Authorization The term authorization refers to the process of getting a medical service(s) authorized from the insurance payer. The term authorization is also referred to as pre-authorization or prior-authorization.
What does referral mean in medical terms?A written order from your primary care doctor for you to see a specialist or get certain medical services. In many Health Maintenance Organizations (HMOs), you need to get a referral before you can get medical care from anyone except your primary care doctor.
Who is issuing the referral authorization?A medical referral is a written order from a primary care physician (PCP) for a patient to be seen by a specialist. A PCP will issue a referral when they believe a patient needs the expertise of another physician for treatment or for testing that needs to be done outside their office.
AUTHORIZATION FORM. Request for additional units. Existing Authorization. Units. Standard requests - Determination within 7 calendar days of receipt of
Patient Referral Authorization FormPresenting symptoms or reason for referral. Pertinent history, findings and specials situations include known discharge needs if inpatient admission. TP-2568.8.
Referrals and Pre-AuthorizationsSchedule your appointment with the provider listed in the authorization letter. If you need to find another provider, contact your regional contractor. Get care